Yes: there’s no doubt that any way we can accurately identify and diagnose early onset psychosis will help patients with mental health disorders with psychotic symptoms. We understand that those words – psychosis and psychotic – elicit strong reactions. The word psychosis can be scary, and the word psychotic can be even scarier. We get it, one hundred percent, because we support families with loved ones with psychosis and disorders with psychotic features every day – and we’ve been doing it for years.
Therefore, we want to share something important. Fear of those words and/or fear of a diagnosis of early onset psychosis is something a person experiencing symptoms such as delusions or hallucinations – and their families – need to face directly, and sooner rather than later.
Why?
Because ignoring symptoms of psychosis creates more problems than it solves, in the long run.
That’s why a study published recently in Nature: Molecular Psychiatry called “Functional Dysconnectivity of Visual and Somatomotor Networks Yields a Simple And Robust Biomarker For Psychosis” might be an important development in our understanding of psychosis, and our ability to identify psychosis before, or soon after, initial symptoms first appear.
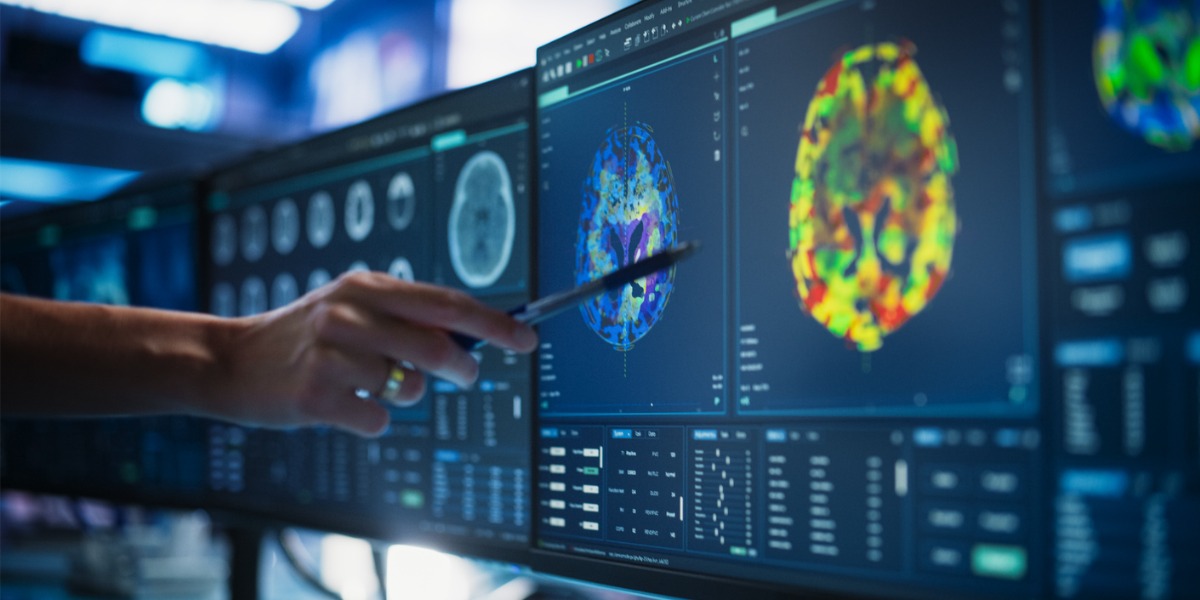
In that study, researchers explored the possibility that scans using magnetic resonance imagery (MR) might be capable of detecting distinct physiological signatures – called biomarkers – in the human brain that can predict the development of psychotic symptoms before they appear.
If the test proves reliable and accurate, and receives consistent verification from additional research teams, this could indeed be a game-changing development.
How We Diagnose Early Onset Psychosis Now
Our current method for detecting psychosis and early onset psychosis is a diagnostic interview, which involves a clinician asking the patient a series of questions about their symptoms, which the patient answers to the best of their ability.
However, while this method works, it has flaws, which mostly revolve around the subjective experience of the patient. For a variety of reasons, a person, especially an adolescent experiencing prodromal psychosis, may not want to disclose the full extent of their experience. Telling another person, in some cases a complete stranger, that you hear, see, and feel things that might not be there can be very scary – and some patients prefer to minimize their symptoms or not discuss them at all.
We understand that, too: no one wants to experience judgment or stigma for any reason. And when there’s risk of judgment, stigma, and discrimination because of something completely out of their control, it’s not surprising that early onset psychosis often goes undiagnosed. That’s a problem, because the duration of undiagnosed psychosis, known as DUP, can have an impact on long-term treatment outcomes.
Here’s how the authors of the study “Effect of Delaying Treatment of First-Episode Psychosis on Symptoms and Social Outcomes: A Longitudinal Analysis and Modelling Study” characterize the consequences of prolonged DUP:
“Treatment delay was associated with impaired recovery in every symptom dimension, with latent harm appearing to develop rapidly during a relatively critical period soon after transition to psychosis, then more slowly as psychosis continued.”
The message from the research is clear: early, accurate detection improves long-term outcomes. In a moment, we’ll share the results of this new study on a potential biomarker for early onset psychosis, detectable by MRI.
First, however, we’ll share several important things to know about psychosis and psychotic disorders, which will help frame and give context for the preceding and subsequent information in this article.
Psychosis: What Patients and Families Should Know
The University of Michigan (U of M) is an important institution for mental health and mental health research in the U.S. Not only do they take a lead role in administering and publishing the annual National Survey on Drug Use and Health (NSDUH), they also regularly publish helpful and informative various mental health topics.
We’ll summarize the essential points of a recent U of M publication on psychosis below. This information will be valuable to our patients with symptoms of psychosis, and their families, as well. It includes core, fundamental facts about psychosis, early onset psychosis, and mental health disorders with psychotic features. We’ll introduce this section with a basic definition of psychosis, as provided by The National Alliance on Mental Illness (NAMI):
“…disruptions to thoughts and perceptions that make it difficult for an individual recognize what’s real and what isn’t. These disruptions are often experienced as seeing, hearing, and believing things that aren’t real or having strange, persistent thoughts, behaviors, and emotions.”
For an in-depth look at early onset psychosis, a description of the various types of delusions and hallucinations associated with psychosis, and a list of the mental health disorders with psychotic features, please visit our treatment page here:
Treatment for Early Onset Psychosis at BACA
Now let’s take a look at the key fact families and patients need to know about this complex mental health condition.
Five Essential Facts About Psychosis and Early Onset Psychosis
1. Psychosis Can Appear in Various Forms
- The first signs of psychosis may be faint voices in the head, the persistent sense that other people want to cause you harm, or seeing things – which may be disturbing – out of the corner of your eye. In some cases, people with psychosis may think someone has access to their internal, personal thoughts, and can monitor, control, access, and add, or remove them their brains.
- In other cases, thoughts, ideas and belief may become completely disorganized and detached from a solid reference in reality. This can lead people with psychosis to become confused, develop unrealistic beliefs, and say things that don’t make sense to anyone else.
- At first, most people understand the delusions and hallucinations aren’t real. However, over time, they can lose perspective, and lost their ability to distinguish what’s real from what’s not real.
2. Psychosis Can Appear Early
- The age of onset of psychosis is wide: between age 14 and age 30. However, patients under 17 do not receive a diagnosis for psychosis, but rather, they receive a diagnosis for early onset psychosis or early onset psychosis.
3. Symptoms Are Associated With Several Disorders and/or Conditions
- The primary symptoms of psychosis are delusions and hallucinations. Delusions are thoughts and beliefs that are objectively and demonstrably false or untrue. Hallucinations involve seeing, hearing, tasting, or feeling things – including people – that aren’t rally there.
- Mental health disorders with psychotic features may include:
- Depression
- Bipolar disorder
- Schizophrenic disorders
- In some cases, people with the following disorders/conditions may experience delusions and/or hallucinations:
- Borderline personality disorder
- Post-traumatic stress disorder
- Autism spectrum disorder (rare)
- Alzheimer’s disease
- Parkinson’s disease
- Age-related dementia
- While the presence of delusions and hallucinations is atypical, it’s possible for people to experience mild symptoms without meeting the criteria for a clinical mental health disorder. Here’s how Dr. Stephan Taylor at U of M describes this phenomenon:
“We didn’t previously accept that people could experience voices or delusions and be perfectly functioning members of society without any distress. Now we see that in some people, it can be just another dimension of human experience.”
- However, in most cases, delusions and hallucinations cause disruption in major life domains and impair the ability to meet basic daily responsibilities associated with work, school, and relationships. That’s why early, accurate detection and timely, evidence-based treatment is essential.
4. Psychosis and Violent Behavior
- There’s a common trope in our society that’s both inaccurate and harmful: the idea that people with mental illness are more likely to become violent, engage in violent behavior, or cause harm to others than people without mental illness.
- In fact, evidence shows that people with mental illness are more likely to be victims of violence than perpetrators of violence: people with mental illness report being victims of violence at a rate 23 times higher than people without mental illness.
- However, the volatility associated with some psychotic disorder means that in some cases, people with mental illness engage in violent acts. Studies – like the one we cite in the preceding bullet – show that violent acts by people with mental illness are most often impulsive, unplanned, and happen in the heat of a crisis moment at home, rather than at locations like work or school.
- That’s another reason why it’s important for families to understand the basic facts about psychosis, and seek treatment sooner rather than later: clear, calm communication from a knowledgeable, supportive loved one can de-escalate a crisis and reduce risk of impulsive, violent behavior. With that said, if anyone experiences a mental health crisis that puts them or others in immediate physical danger, please call 988 or 911, explain what’s happening, and keep yourself and the person in crisis safe until help arrives.
5. Treatment For Psychosis is Effective
- The American Psychiatric Association (APA) indicates that Coordinated Specialty Care (CSC) is the most effective approach to treating psychosis in adolescent and young adult populations.
- CSC is a multidisciplinary approach that includes:
- Psychotherapy: cognitive behavioral therapy for psychosis (CBTp)
- Medication: typical and atypical antipsychotics
- Case management: people with psychosis experience better outcomes when a case manager oversees their treatment journey
- Family support: when families understand the facts about psychosis and psychotic symptoms, they can support their loved ones in a healthy and effective manner
- Peer support: in some cases, meeting and talking to others with a similar experience can reduce isolation, engender hope, instill optimism, and improve outcomes
- Lifestyle changes and education: classes and workshops on healthy eating, exercise/activity, stress management, sleep hygiene, conflict resolution, and how to form and maintain healthy relationships can help improve overall daily functioning for people with psychosis
That’s the end of our list of essential facts for people with psychosis and their loved ones to know and understand. We hope you got the message that we began stressing in the beginning of this article: early, accurate diagnosis and timely treatment can dramatically improve long-term outcomes, and help people learn to manage the symptoms of psychosis and successfully engage in the basic functions of daily life.
Now let’s look at the study we mention above and learn whether the research team found a way to improve how we diagnose early onset psychosis.
Detecting A Biomarker for Early Onset Psychosis With Magnetic Resonance Imaging (MRI)
In this study, researchers examined MRI scans from 105 patients with symptoms of psychosis and compared them to MRI scans from 54 patients with no symptoms of psychosis. Here’s what the scans showed:
- Patients with psychosis showed hypoconnectivity – meaning fewer connections than typical – between areas of the brain associated with sensory input and the cortex.
- Patients with psychosis showed hyperconnectivity – meaning more connections than typical – between the cortex, the thalamus, and the somatomotor (movement) and visual networks in the brain
- The same patients did not show hyperconnectivity in primary auditory and visual networks in the brain
- The somatomotor-visual biomarker was unique to patients with psychosis, and was not impacted by the presence of other psychiatric comorbidities, including substance use, nicotine use, stress, anxiety, ADHD, or demographic variables.
Here’s how Dr. Brian Keane, professor of neuroscience at the University of Rochester and lead author of the study, characterizes these results:
“Establishing such biomarkers could provide a key step in changing how we care for, treat, and offer interventions to people with psychosis. A single five-minute scan could potentially improve our ability to predict which at-risk individuals will transition to a psychotic disorder, which in turn could allow for more timely treatments or interventions.”
At BACA, we welcome any new development that can improve treatment outcomes for our patients. With regards to early onset, prodromal psychosis, a test for a biomarker could improve the diagnostic process by making diagnosis faster, easier, and more reliable. Because the marker is an effective measure regardless of the presence of other mental disorders, it can eliminate the guesswork that can occur when a patient appears with symptoms that overlap with more than one diagnosis.
In addition, the presence of an objective biomarker can remove the uncertainty associated with diagnostic interviews that depend on memory and effective communication. In cases where a young person does not understand what’s happening with their own thoughts, behavior, and emotions, they may not be able to describe their symptoms in a way that’s clear to a provider, and they may not understand that what they really need is professional support.
A biomarker for psychosis can change that, and allow providers to arrive at an accurate diagnosis, and allow patients to initiate treatment early, which evidence conclusively shows improves long-term outcomes for people psychosis.